You are sitting at lunch at your desk, worrying that the report you just finished isn’t good enough. You know about the benefits of self-compassion and wonder if practicing it would make you feel better about your work.

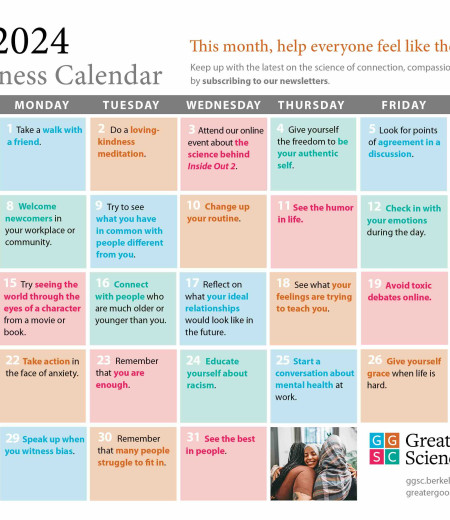
For example, there is one self-compassion exercise where you think of something that bothers you about yourself. You then write a letter from the perspective of a compassionate friend. There’s another exercise in which you imagine a compassionate friend comforting you as you struggle. And there’s an exercise meant to tackle the self-critical voices in your head.
You could use a compassionate friend right about now to reassure you about your report. You imagine a friend sitting next to you, saying words of reassurance: “It’s OK, you did your best on the report and that’s all you can ask of yourself. It will be fine.”
But your friend’s imagined words feel empty. You don’t feel any better. In fact, you feel worse; now you are thinking about that time you turned in a report that your boss thought was terrible. You are now even more convinced your report is bad.
In doing these mental exercises, you have just experienced what self-compassion researchers call “backdraft.” Backdraft happens when you try to be compassionate to yourself and end up feeling worse. “It’s a normal part of practicing self-compassion,” says Chris Germer, a clinical psychologist and lecturer at Harvard Medical School’s department of psychiatry who, with Kristin Neff, developed a program called Mindful Self-Compassion.
What can you do if practicing self-compassion makes you feel worse, or if the thought of being loving toward yourself is off-putting? Luckily, there are other ways of caring for yourself when you’re struggling that don’t always involve thinking warm, reassuring thoughts in your head.
When self-compassion backfires
Fear of or aversion to self-compassion can arise in those who grew up with insecure attachment to our parents—some 40% of us. In secure parent-child relationships, caregivers are consistently appropriately responsive to the child’s needs. The securely attached child grows up with a sense of safety. With insecure attachments, parents are not consistently and appropriately responsive to the child’s emotional cues. A parent may be too disengaged, angry, or depressed too often to respond well. These children grow up with a degree of anxiety about the world.
Paul Gilbert, a clinical psychologist and the founder of compassion-focused therapy, first explored the relationship between attachment style and fear of self-compassion. He described how two emotional regulation systems, what he called the contentment system and the threat system, develop differently if we are securely attached versus insecurely attached.
The contentment system, as he calls it, in securely attached children gives a child a sense of support from others. This creates emotional memories of feeling secure and supported that can then be activated by self-compassion. Because thoughts can trigger emotional memories, merely thinking of a compassionate mother’s hugs can soothe adults who were fortunate enough to receive them.
Insecurely attached children do not receive that sense of safety and reassurance from their caregivers. They don’t have the same stock of comforting emotional memories that become activated during the practice of self-compassion.
Worse, insecurely attached children have highly active threat detection systems, Gilbert explains. A gesture of compassion that an adult who was securely attached would find comforting, a child of insecure attachment could find threatening.
For example, say the child of rejecting parents experiences sadness. Instead of meeting that sadness with compassion, the parents of the insecurely attached child dismiss the child’s sadness with a scowl and tell her to toughen up. This experience of rejection threatens a child’s sense of social safety. The threat system is activated.
Children with active threat systems can come to see the need for compassion as a sign they are weak. Here’s how it works: A child who requested compassion from their parents—by crying, say—and was met with disgust at their weakness for needing compassion becomes an insecurely attached adult who is not receptive to compassion, whether offered by self or others. Say this insecurely attached adult is feeling sad and a friend approaches to offer compassion. The insecurely attached adult recoils from the offered compassion, thinking that the friend must be seeing them as weak. After all, it is only weak people who need compassion; the person offering them compassion is really implying they aren’t tough enough to handle the situation.
These adults “resist any expression of compassion due to concerns of being rejected, harshly criticized, or feeling undeserving,” write Derricka Boykin and her colleagues in a 2018 study.
Gilbert devised a survey to measure how intense the fear of self-compassion can be. By looking at the different statements on the survey, we can get a sense of the different fears people have about self-compassion. These include:
- “I fear that if I become kinder and less self-critical to myself my standards will drop.”
- “I fear that if I become more self-compassionate I will become a weak person.”
- “I fear that if I become more compassionate toward myself, others will reject me”
For those who tend to score high on the fear of self-compassion—like the grown children of insecure attachments, as well as survivors of abuse and women with eating disorders—doing mental practices, like sitting down at lunch to practice a Self-Compassion Break, might not be the best approach.
An alternate way to practice self-compassion
Mental practices can be re-traumatizing, Gilbert says. Specifically, say, you try to help yourself by saying it is OK to feel sadness. Instead of feeling comfort from your words to yourself, you start to feel anxious because you have an emotional memory of being told that sadness is unacceptable (even if you aren’t conscious of it).
The alternative is to practice behavioral self-compassion, or figuring out what you need in the moment to feel soothed—for example, petting your dog or taking a short break from work.
“Everyone needs to customize self-compassion practice for their own, individual needs and life circumstances,” says Germer. “As a rule of thumb, behavioral self-compassion is safer than mental exercises.”
When we are upset, though, it can be difficult to practice behavioral self-compassion and figure out what we need in the moment. Germer recommends asking specific questions: What do I need to feel safe? To be comforted, soothed, validated? To protect, provide for, motivate myself?
Germer advises us to think about how we already care for ourselves and try applying those practices. For example, you might care for yourself physically with exercise or a warm bath. You might care for yourself mentally by watching a funny movie. You might care for yourself emotionally by journaling or cooking. See this worksheet for these suggestions and more.
Of course, it is not always easy to soothe yourself in the way that is best for your well-being. How many times have you really wanted to eat a cookie because you were stressed, but were able to step back and say, “I should take a warm bath instead”? It is hard to do.
Yes, it can be hard for us to figure out what we need in the moment and choose a healthy path forward when practicing behavioral self-compassion, Germer says. “We can’t become more self-compassionate overnight. It’s a practice that takes time. The more we practice, the more self-compassionate we become.”
When you are reflecting on what you need, he suggests, you might ask yourself again what you really need in the hopes of heading off some less salubrious choices.
These behavioral practices are best for when you need to establish a sense of safety in your practice of self-compassion. Psychological safety is feeling that you can put forth your ideas, make mistakes, and take risks without worrying that you will be humiliated or ridiculed.
Once you are feeling safe—where you feel you won’t be attacked—it may then be the right time to move on from the behavioral exercises alone to also tackle the mental exercises. But maybe not by yourself at your desk.
Self-compassion together
If you are going to try self-compassion exercises when you are alone, research suggests you might want to do them in front of a mirror. In one study, reciting compassionate phrases in front of a mirror proved more powerful than reciting the phrases without a mirror. Researchers speculate this is because the mirror allows us to see our face and eyes, which are important in the way we communicate compassion.
But it is best not to practice alone at all. “We say that self-compassion is a ‘team sport,’” says Germer. “Although it’s called ‘self’-compassion, it’s best learned in community.” When we see others meeting some of the same obstacles that we have and how they overcome them, we are better able to do the same. Self-compassion programs are an excellent way to practice in a community.
But, Germer says, there is a trick to practicing self-compassion. The best advice won’t help you if you do not practice self-compassion with the right intentions. Here’s how to think about practicing self-compassion with the right intentions:
“When we suffer,
we give ourselves compassion not to feel better,
but because we feel bad.”
“Trying to practice self-compassion to manipulate our moment-to-moment experience will ultimately fail,” Germer says. “People need to be guided into practicing for its own sake, as we might care for a child with the flu, not to drive out the flu but as a simple expression of sympathy and kindness.”






Comments