The Bayview Child Health Center is set back from Third Street, the chief thoroughfare in San Francisco’s Bayview-Hunters Point neighborhood. The street is lined with weathered pawn shops, check cashing outlets, small liquor and grocery stores, and bars. People in janitorial or business attire wait for public transportation to jobs downtown, while young men and women in baggy hip-hop gear hang out on the corners. Bayview-Hunters Point has the highest concentration of families in San Francisco, but the Bayview Child Health Center is one of only a handful of pediatric clinics in this neighborhood.
Geographically isolated from the rest of San Francisco, a hot spot of violence and crime, beset by toxic hazards from the neighborhood’s shipbuilding industry, Bayview’s largely African-American community is struggling with a range of health problems. A 2004 health assessment by the city of San Francisco showed more heart failure, asthma, ambulance use, and low-birth weight babies in Bayview than in any other neighborhood in the city. The infant mortality rate in Bayview is the highest in all of California.
But the poor health of Bayview’s residents can’t just be attributed to violence, poor air quality, lack of adequate medical care, and other physical hazards. They face another danger, one that’s harder to quantify but perhaps no less harmful to their health: a chronic sense of powerlessness.
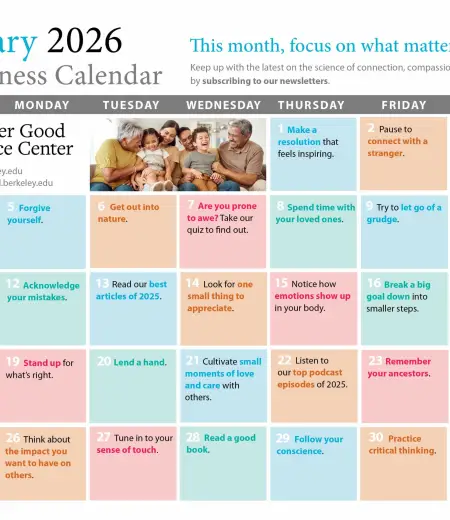
 Nadine Burke at work in San Francisco's Bayview Child Health Center. "Power plays a huge role in my work," she says.
© Bill Posner/California Pacific Medical Center
Nadine Burke at work in San Francisco's Bayview Child Health Center. "Power plays a huge role in my work," she says.
© Bill Posner/California Pacific Medical Center
According to Nadine Burke, the medical director of the Bayview Child Health Center, to live in Bayview is to feel that you’re not in control of your destiny, that your neighborhood is socially and economically weaker than surrounding communities.
“Power plays a huge role in my work,” says Burke. “The messages here daily, all the time, are that you are not important and you have no power. When you are exposed day after day to poor living conditions, violence, and environmental injustice, you start to feel like you are not important and that your voice is not being heard. It’s easy to feel like you don’t have any power.”
Research has linked such feelings of powerlessness to the kinds of health problems plaguing Bayview and many other communities around the world. This research shows that members of poor communities do not merely experience higher levels of violence; they are also more likely to have high blood pressure and frequent periods of increased heart rate, which contribute to a higher mortality rate. What’s more, similar health problems have been shown to afflict the least powerful members of nonhuman primate species.
Taken together, these and other findings suggest that the psychology of powerlessness can wreak havoc on people who sit low on the totem pole of any social structure.
“Poverty, and the poor health of the poor, is about much more than simply not having enough money,” says Robert M. Sapolsky, professor of neurology at Stanford University. “It’s about the stressors caused in a society that tolerates leaving so many of its members so far behind.”
The agony of powerlessness
Sapolsky’s research has been critical to uncovering the link between a sense of powerlessness and long-term health problems. In a series of studies, Sapolsky and colleagues found that baboons and other nonhuman primates low in their troop’s social hierarchy face constant threats of petty violence and bullying from those above them. Their bodies respond to this stress by releasing the hormone cortisol, which gives the body an extra shot of energy, useful for short bursts of running or brawling—the so-called “fight or flight” response.
What’s more, Sapolsky argues, primates can turn on stress responses for purely psychological reasons. We remember previous threats and are plagued by the lingering fear that an attack could come at any time. In a primate who’s been victimized in the past, even mild teasing can trigger a disproportionate stress response, such as a big shot of cortisol.
While cortisol might help primates confront or avoid immediate danger, it also increases blood pressure and blood sugar levels, and weakens the immune system. As a result, continuously stressed-out primates are at much greater risk for diseases like hypertension, inflamed arteries, and insulin-resistant diabetes, and are more susceptible to problems with their immune and reproductive systems, as well as psychological disorders.
Humans may not face the threat of bloody violence as frequently as low-ranking baboons, but there are plenty of other ways we can feel disempowered. Worldwide, many studies have documented health disparities not only between the affluent and the poor but between the educated and the less-educated, ethnic majorities and minorities, and other groups defined by power imbalances. In each case, members of the disadvantaged group have shorter life spans when compared with more powerful members of society. African-American men, for example, are three to four times more likely to suffer strokes than white males.
Other research corroborates that this is not merely a function of environmental factors such as reduced access to health care or fresh food. When Harvard University’s Ichiro Kawachi and colleagues analyzed a two-year slice of United States Census data, covering the deaths of almost 400,000 people, they focused on death by diseases with no known methods of prevention, treatment, or cure. Since no amount of money could buy freedom from these diseases, Kawachi assumed they might affect the powerful and powerless equally, without regard to income. Yet his results suggested otherwise: Those who were lowest on the socioeconomic ladder were more likely to die—even though the ability to afford and access health care should have conferred no advantage. This suggested to Kawachi that feelings of power might have more of an impact on heath than the material benefits associated with high income.
While Kawachi and his team used socioeconomic status as a marker of power, additional studies have revealed that health disparities can be rooted in feelings of discrimination. Vicki Mays, head of the UCLA Department of Minority Health, argues that the perception of discrimination, as well as actual discrimination, can affect health just as strongly as sitting low on the socioeconomic ladder—with negative effects similar to what Sapolsky discovered among baboons. In a paper published in the 2007 Annual Review of Psychology, Mays and her co-authors review a range of evidence showing how perceived discrimination can activate the stress response, which translates into poor health for the victims of that discrimination. They report, for example, that compared to white American women, even African-American women at the high end of the socioeconomic ladder are at higher risk of delivering low-birth-weight babies.
The stress of discrimination can also lead to risky behavior. When a team of epidemiologists in four American cities followed 3,300 black and white adults over a period of 15 years, they discovered that 89 percent of blacks and 34 percent of whites reported that they had at some point felt discriminated against, and that those people were far more likely to engage in risky behavior such as drinking, smoking, and using illegal drugs.
The study also found that affluent and educated African Americans were more likely to report discrimination, while the reverse was true for whites. “That makes sense,” says Luisa N. Borrell, lead author of the study and professor of epidemiology at Columbia University, “because African Americans who are poor are more likely to interact with people who are like them.” But if you are a black person in a predominantly white environment, she adds, even with a higher income you might feel singled out and thus more sensitive to discrimination. Meanwhile, whites at lower income levels are often in the minority in their communities, and thus “get a double hit,” feeling both poor and out of place.
Robert Sapolsky points out that low socioeconomic status and racial discrimination often work in tandem to create similar effects: “Both low socioeconomic status and racial discrimination tap into the same corrosive elements of psychosocial stress, namely lack of control and predictability, lack of coping outlets, and a static system that allows little room for optimism.”
As this research suggests, there’s no simple formula to determine a person’s level of power. It’s not as easy as looking at any one factor, such as socioeconomic status, since feelings of personal power are shaped by a variety of subjectively experienced social and environmental forces. Social status, says Borrell, is in the eye of the beholder. “You’re affected by looking at how far you are from the person next to you on the ladder,” she says. “That’s what creates stress.”
To support this claim, Borrell points to research on the connection between income and personal happiness. A 2005 study by sociologists Glenn Firebaugh and Laura Tach has found, for instance, that a person’s reported level of happiness in the U.S. depends less on one’s income level than on how one’s income compares to that earned by others in the same age group. Wide disparities in income can make people unhappy and stressed out, even when absolute incomes are relatively high.
Making it work
What can be done to address these health disparities? Borrell argues that there is only so much health professionals can do because the nature of the problem is political and societal. “It is something that is beyond the individual level. It needs to be addressed by the structure of the society,” she says.
Harvard’s Ichiro Kawachi agrees. He identifies a range of social policies that would be vital to promoting greater socioeconomic equality—and hence, better health. “Make an investment in education, for example, to give people a decent start in life,” he says. “We can subsidize childcare, which is a major stress for low-income mothers, especially those who are single parents. We can expand unemployment insurance and expand access to health care. This is controversial only in the United States. Other societies view health care as a basic human right.”
Kawachi says that to address health disparities, health professionals must go beyond their offices and clinics and enter the realms of social and government policy. “Health professionals ought to be among the first to go out there educating politicians, policymakers, and the public. There’s only so much that medicine can do in putting bandages on people. The fundamental causes of health disparities in our society are failures in social policy.”
This approach is embraced by Nadine Burke, whose work does not end at the Bayview Child Health Center. She participates in countless hearings, commissions, and planning sessions—and she is passionately committed to having a clinic that reflects the composition and needs of the surrounding community.
Burke emphasizes that to address health disparities that flow from differences in power, the community itself must set the agenda for change. She points to a “disconnect” between community members and the experts who study them, whose recommendations and treatments can exacerbate feelings of disempowerment. “The people who are involved in trying to find solutions are not necessarily the ones who are able to understand the problems in a way to properly address them,” she says.
While Burke works to empower the community from her medical office, community activists like Espanola Jackson, sometimes known as “the mother of Bayview,” are trying to change the balance of power in their neighborhood. For 30 years, Jackson has led campaigns on issues from affordable housing to rallying for educational and professional training opportunities. Today, her primary fight is to clean up the toxic and radioactively contaminated shipyard in Bayview, which has sickened many Bayview-Hunters Point residents.
Jackson has seen a sense of powerlessness take its toll on the health of the community—and to her, the path to better health requires overcoming apathy and building political power. “Everyone must stop sitting back and letting the politicians tell them what is good for you,” she says, noting that only 20,000 people vote out of a pool of 60,000 potential voters in Bayview. To improve the health of Bayview, says Jackson, “We need that power.”
Burke knows the problems that arise from powerlessness will not end overnight. She sees her work as part of a long-term effort to build the power of the community. “It is important to have our clinic here in the Bayview, where there has been so much poverty and hopelessness,” she says. “One of the most important things I can do is stay here and make it work. I think that sends a powerful message that we value our families enough to make sure that we bring the highest quality resources here, because they deserve it.”



Comments