As a hospice volunteer, I once asked a woman I’d been visiting for several months what she wanted for her upcoming 75th birthday. She was wheelchair-bound, living in a nursing home, and in the last stages of metastatic breast cancer.
“Life,” was her answer.
Life. Of course. We all want to live as well and as long as we can. Eventually, though, our bodies betray us and we begin to show the telltale signs of aging. And, as we age, we have to reconsider and accept who we are now, and think seriously about how we want to live throughout our last chapters.

No one wants to think about the prospect of death. But as we lurch into old age, we are faced with the prospect that many of us will need what our medical system does not currently provide: high-quality end-of-life care. It’s more than a personal concern; it’s a pressing societal issue. Projections are that, by 2030, one-fifth of the population will be 65 and older, compared to 13 percent in 2015, and 9 million people will be over 85.
Currently, our country’s end-of-life care is fragmented, costly, and unsustainable. Too much aggressive care is given that is futile and ruinous to people’s quality of life. Doctors frequently don’t discuss with patients and family what truly matters to them and offer comfort; and those left behind are often wracked by a sense of guilt, haunted by the choices they’ve made in the heat of the moment without really knowing their loved one’s wishes.
Fortunately, there are people, places, and organizations that are taking a serious look at how to improve quality care, and some are making strides in the right direction.
In my book, Last Comforts, I chronicle the current realities of end-of-life care, and point to some of the outstanding pathfinders and innovations in this field that could make a difference for all of us. It’s not just about “brink-of-death” care. It’s about how to better educate doctors and nurses; provide more effective dementia care, design and operate better long-term care facilities, recognize the unique challenges of minority and LGBT people, and provide better training and a living wage for the nursing assistants and home health care aides who do so much of the hands-on care for elders. Ultimately, we need to understand how public policy decisions about palliative and hospice care affect us.
What can we do as individuals? The first, and probably the toughest, task is to look our own mortality squarely in the eye. That’s no easy feat, and certainly not encouraged in our death-denying culture. But if we do, we can be better advocates for ourselves—and our loved ones—and can begin to understand the many choices we will have to face, and take some responsibility for ensuring our wishes are met.
Here are some of the lessons I’ve learned—from my experience as a hospice volunteer, as well as from my research as a reporter—on how people can prepare better for the end of life:
1. Educate yourself about the different key treatments for end-of-life care, so that you can make informed decisions
Before we can talk to our family or friends about what matters to us and what we’d want at the end of our lives, we have to think about it seriously—and get better educated about it.
These are profound questions about the very heart of our lives: If you had a limited amount of time left to live, what would be most important to you? What would make life continue to be worth living? What would you be willing to tolerate, in terms of rigorous and aggressive treatment, in order to achieve a longer life?
That’s the framework for looking into the many tools that hospitals have at their disposal to prolong life, and how those tools may be employed at critical moments. It helps to know in advance what these life-saving procedures actually look like in practice, so you can better assess which, if any, would be acceptable to you, and under what conditions.
If you’ve never had to consider these kinds of aids before, it can be difficult to envision. You may just end up relying on your doctor’s recommendations or, more problematically, movies and TV portrayals, where unrealistic outcomes are the norm.
CPR, advanced life support, intubation, and feeding can be life-saving, particularly when you are young and have an acute condition. But, for the elderly, they can often significantly decrease quality of life without providing much benefit. For example, many doctors will prescribe feeding tubes to patients with dementia, even though it can lead to pneumonia, infections, and ulcers, and may not prolong life much.
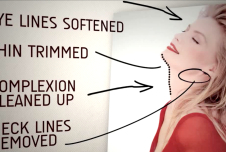
To better decide for yourself, it might help to read about these procedures, or to even watch videos that show what the treatments involve, which you can find here.
2. Start conversations with loved ones so that they are clear about your wishes for care

If you’re clear about what you value and how you’d want to be cared for toward the end of your life, don’t keep it a secret! This is the time to have a conversation with your loved ones about what you want—particularly critical guidance for them if you are in a medical crisis and cannot speak for yourself. And bear in mind that this is not a one-time conversation. Your own feelings may change over time, depending on your circumstances, and if they do your loved ones need to know.
Nobody wants to talk about these things. How do you start? Remember when our children were younger and we looked for “teachable moments” to discuss pressing issues? I believe in looking for “teachable moments” for talking about serious illness and end-of-life issues, too. If a friend of the family or the parent of your child’s best friend is going through a medical crisis, for example, it might be a perfect time to turn the conversation to your own family, and your own thoughts and feelings on the matter.
If you need a good prompt, The Conversation Project offers useful “starter kits” to kick off a discussion, including one for those suffering from dementia.
If you cannot speak for yourself in a medical crisis, an advance directive and a designated health care proxy will help to navigate the system more smoothly on your behalf. Choose a health care proxy who not only understands what you want, but is willing and capable of carrying out your wishes. You can find advance directive forms for each state at Caring Connections, a program of the National Hospice and Palliative Care Organization.
3. Understand the benefits of palliative care and hospice care and know when to ask for them
Palliative care is a medical specialty that is available to anyone with a serious illness, whether or not you are dying. Palliative care addresses your symptoms, whether they’re physical, such as pain or nausea, or whether they’re emotional or spiritual. Interdisciplinary teams of caregivers including doctors, nurses, and social workers are dedicated to providing coordinated care that plans your care based on your goals and values. And you can still receive curative care concurrently. Palliative care may or may not lead to hospice care; but it will allow you to decide how you want to be cared for over time as your illness progresses.
Research suggests that palliative care is an important factor in determining how families rate the quality of end-of-life care received by loved ones. In one study, cancer patients who were randomly assigned to receive early palliative care versus standard medical care reported better moods and quality of life throughout treatment, and they lived longer on average, even though they received less aggressive treatments. A recent review of research found that, for oncology patients, early palliative care improves quality of life, “mood, treatment decision-making, health care utilization, advanced care planning, patient satisfaction, and end-of-life care.” It also may improve symptoms and survival.
Hospice care differs from palliative care in that it provides comfort care only if your illness is life-limiting and you have a prognosis of six months or less, and you must forgo any treatments aimed at curing the illness. Hospice care is provided mostly in people’s own homes (and that includes assisted living and nursing facilities), but can also be provided in a hospital, or in a dedicated hospice facility. Though some people avoid hospice because they (mistakenly) believe that it means “giving up,” at least some research suggests that hospice patients are more likely to live as long (or longer) than terminally ill patients in hospitals.
Both of these services can make a tremendous difference in the experience of facing a terminal illness. Just having a say in one’s care and knowing that medical staff and loved ones understand your wishes can be a huge relief.
4. Learn how to communicate effectively with doctors and medical staff
Many doctors are far better at the art and science of medicine than they are at actually communicating with patients. And yet, if you have a serious illness and have to make informed decisions about your care, you want someone to communicate your choices, the risks and benefits of treatment, and the pros and cons of different options, as clearly as possible. Your doctor should be comfortable talking to you about end-of-life wishes in an honest, meaningful way, and listen, show empathy, and encourage questions. Research has shown that patient satisfaction goes up when doctors employ these types of skills, and they can have an impact on outcomes as well.
Be prepared to ask questions about recommended medications or surgeries and their side effects, alternative therapies, and the anticipated outcomes of treatment versus no treatment. Too often we leave the office without this vital information and end up making decisions for expensive and futile treatments that do little to prolong life and can have serious consequences on the quality of the life left to us.
It’s often helpful to bring along a supportive family member or friend to a doctor’s appointment to take notes; or, if that’s not possible, to record your conversations with your doctor. That way, if you receive bad news and find yourself overwhelmed with emotion, you’ll have the important information written down or recorded to refer to later once you’re feeling calmer.
5. Research nursing and assisted living facilities in your community, in case you need them
I’d bet that nobody ever thinks, “Gee, when I get older, I really want to go live in a nursing home.” We’d prefer to remain independent and age in place in our own homes. And, indeed, more options are becoming available for that to happen. This is encouraging, since reports suggest that aging in place can have emotional and health benefits for those who can manage it.
But, for some of us, end-of-life care may involve assisted living or nursing home care, especially if we live long into old age. Not all of us will have supportive family and friends available to care for us if we need help. Many do not have adult children; or have adult children who live too far away to provide daily care. Luckily, there are some innovative long-term care developments that offer patient-centered care. That means that you spend your day according to your schedule, not an institution’s: rising, dining, dressing, and participating in activities as you choose. Moreover, there’s much to be said about living with others in a setting that can combat the loneliness and isolation that afflict so many elders living alone and that contribute to poor health.
You can learn more about culture change and patient-centered care in long-term care settings from two organizations, The Pioneer Network and LeadingAge. The Pioneer Network offers a list of excellent questions to ask if you’re considering a move to assisted living. You can also compare quality of care in a nursing home by checking Medicare’s Nursing Home Compare website, and looking at their guidebook for how to assess staffing, operations, and care at a nursing home.
6. Advocate for better end-of-life care for everyone
 This essay is adapted from Last Comforts (Cypress Publishing, 2016, 350 pages)
This essay is adapted from Last Comforts (Cypress Publishing, 2016, 350 pages)
In addition to planning for our own care, I can’t emphasize enough how important it is to advocate for everyone. Our current system is plainly unsustainable. I believe that for aging baby boomers, it’s time to tap back into our activist genes and address the many intertwined social and medical issues involved in end-of-life care.
The very foundation of how society pays for palliative care should be rethought and adjusted to respond better to the way people really die now (as opposed to how they died in the ‘70s, when hospice began). The way we deal with multiple cultures and differences in sexual and gender orientation has to become more sensitive. The way we design and operate long-term care facilities has to change to better enhance the dignity and quality of life of their residents. The way we train and compensate direct care workers, such as certified nursing assistants and home health aides, needs to reflect the growing importance of their role. The way public policy addresses medical care but not the critically important element of non-medical support for the very frail has to change, too.
In the medical realm, we can support initiatives aimed at compensating professionals who go into palliative care fields. It’s still too often the case that tests, procedures, and treatments are reimbursed at a higher rate than are the compassionate discussions with patients and their families that are the heart of good end-of-life care.
We can also support research into palliative care. Too few studies have looked at some of the important elements of care, like how much palliative care is tied to pain reduction, cultural issues, spiritual issues, or even patient satisfaction with the process.
We must do all what we can to arm ourselves with knowledge, to communicate clearly with others about our wishes, and to advocate for quality end-of-life care. Our lives, literally, depend on it.







Comments